The incidence of large intestine cancers is increasing all over the world, including in India. Much like any other cancer, if the diagnosis is early, colorectal cancers (CRCs) can be cured. Unfortunately in India, diagnosis is generally late, with patients coming in only at the advanced stages, at which point, only palliative care and treatment is possible.
Understanding colorectal cancers
CRC ranks as the third-most prevalent cancer globally, and is the second primary cause of deaths associated with cancer around the world. In the United States, CRC ranks as the second-most common cause of cancer-related deaths, following lung cancer. Many CRC cases however, are preventable. The American Association for Cancer Research observes March as Colorectal Cancer Awareness Month in order to raise awareness about the disease.
We, in India, need to follow this example, as CRC is the fourth-most common cancer in India for both sexes, and one of the six most common gastrointestinal cancers in India. Despite the incidence of colorectal cancer (CRC) being low in India compared to the West, it is a leading cause of cancer deaths here. If patients report early to a doctor, CRC can also be cured. Unfortunately, as is the case, reporting to the physician late in an advanced stage severely limits the kind of interventions medicine can provide.
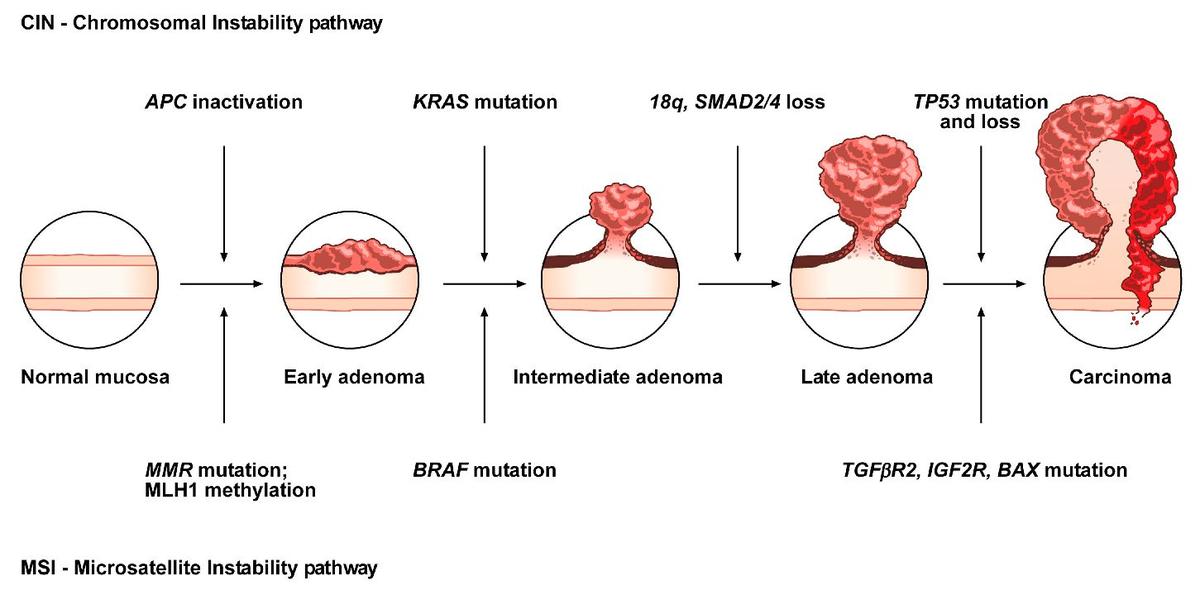
Source : ‘The Molecular Hallmarks of the Serrated Pathway in Colorectal Cancer’ – Cancers 2019 Jul 20;11(7):1017. doi: 10.3390/cancers11071017)
Why is there a need for awareness?
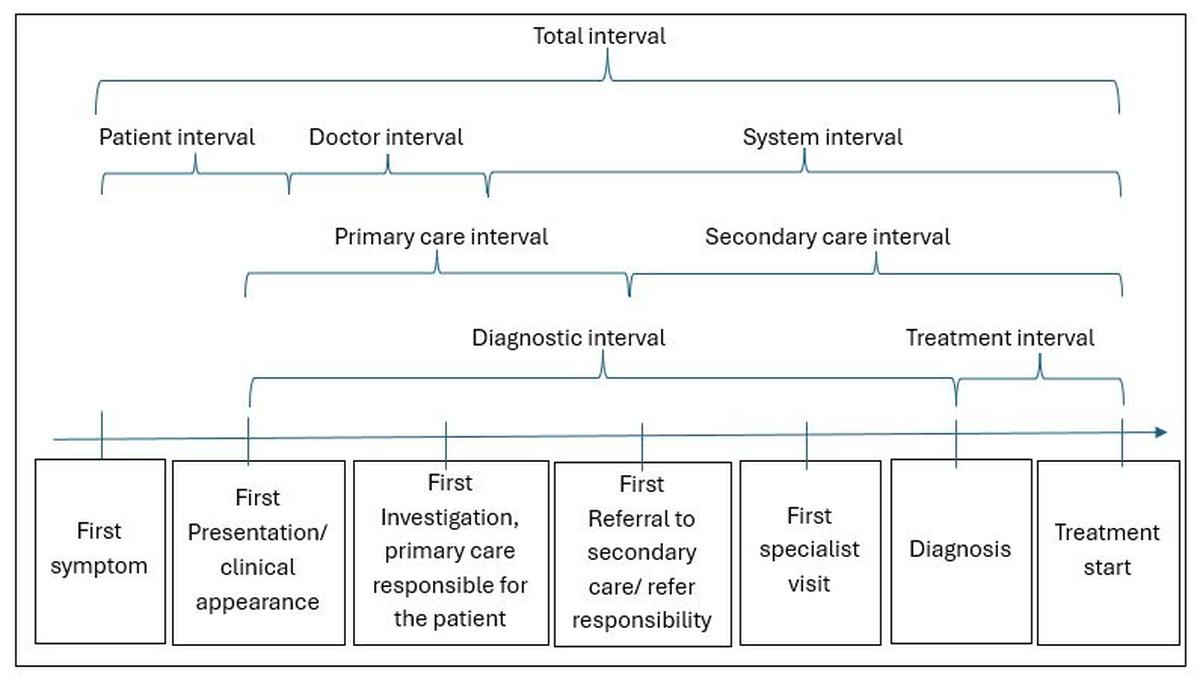
In order to understand the need for awareness one needs to understand the intervals in healthcare. People often ask doctors why there is an awareness month, or talk, or media information, when they are ready to consult a doctor if they become symptomatic. To explain this, one needs to understand three types of intervals: disease interval, diagnosis interval, and treatment interval.
Disease interval is the time a disease takes to manifest: it may remain silent at an early stage and cause symptom(s) later in an individual, urging him/her to report to a doctor. The diagnosis interval is the time taken from a patient presenting with symptoms to the final diagnosis. Unfortunately, symptoms can be vague, non-specific, and common to many diseases, challenging even an astute clinician and specialist, and potentially delaying the diagnosis. The third interval is the ‘treatment interval’. This is the time taken by the patient to begin the right treatment. If all these three intervals are taken care of wisely and remain short, the disease outcome is most likely to be favourable. Public awareness about these intervals therefore, is essential and to do so becomes the responsibility of the medical fraternity and media in every society.

To explain this further, I would like to bring in three real-life case scenarios.
Example 1: An elderly person aged above 65 felt very weak and was found to have low haemoglobin (anaemia), and so he started taking iron supplements on his own. When he didn’t show much improvement and felt weaker, he agreed to go in for detailed investigations. A colonoscopy examination revealed a malignant growth (cancer) of the caecum (lowermost part of the right side of the colon), which is notorious for presenting as anaemia to start with. In this case, both disease and diagnosis intervals were stretched out, but luckily, he underwent surgical treatment immediately without further delay, and the outcome was optimum.
Example 2: During the COVID-19 pandemic, many patients did not report to hospital for non-COVID symptoms for fear of contracting COVID-19. To resolve this issue, we developed a web link for the public to self-assess the seriousness of non-COVID symptoms through a scoring system, consultdocnow.com, to guide them in consulting a doctor at an appropriate time. A 70-year-old lady with habitual constipation, suffering from severe constipation for three months, reported to our emergency department during the Covid pandemic after referring to the weblink, with severe abdomen pain and abdominal distention. On colonoscopy examination, we found obstructive cancer on the left side of the large intestine, which was relieved with lifesaving endoscopic stenting. Unfortunately, an advanced scan (PET scan) revealed the spread of cancer due to a delay in consulting a doctor.
Example 3: A 47-year-old executive had rectal bleeding, which he presumed to be due to haemorrhoids (piles) and so he self-medicated. When he started experiencing a recurrence of bleeding, he underwent a colonoscopy, which revealed cancer of the rectum in addition to piles. Subsequently, he was treated for both. Here, the delay again, was due to a lack of awareness.
These case scenarios highlight that intervals from disease initiation to treatment can often be long, underscoring the need for awareness about colon cancer.
Source: Journal of Neuro-Oncology 18(3), 445–454, 2016 doi:10.1093/neuonc/nov187 Advance Access date 1 November 2015)
What is the screening process for CRC?
Colorectal cancer awareness is vital because screening of the colon by colonoscopy can help prevent this cancer by identifying precancerous ‘polyps’ (fleshy lesions arising from the mucosa of the large intestine) during the procedure, and can be removed at the same time. Left alone, these polyps can grow in size over the years and turn into cancerous lesions. Furthermore, colonoscopy can also detect CRC in the early stages, when treatment is more likely to be successful.
A colonoscopy is an endoscopic examination of the inner lining (mucosa) of the entire colon and rectum. It is usually done after a thorough preparation of the colon under intravenous conscious sedation and is painless. The colonoscopy examination of the large intestine, called ‘screening colonoscopy,’ remains the cornerstone of early diagnosis of CRC.

CRC awareness also emphasises the greater use of at-home screening tests like Cologuard (a stool DNA test that screens for colorectal cancer) and FIT (a Fecal Immunochemical Test) to detect blood in stool, which is one of the markers for CRC.
What are the risk factors for CRC?
The age-standardised incidence rate for CRC in India is between 4 and 6 per 100,000 men and 4 to 5 per 100,000 women. In 2022, India had 64,863 cases and 38,367 deaths from CRC. The five-year prevalence of CRC in India is estimated to be 87 per 100,000 people.
Risk factors include being over the age of 50, a family background: a first-degree relative diagnosed with colon cancer or polyps; a personal history of having polyps; inflammatory Bowel Disease (IBD) and genetic cancer syndromes: Lynch syndrome (Hereditary Nonpolyposis Colorectal Cancer) and Familial Adenomatous Polyposis (FAP).
Adjustable risk factors include obesity due to a sedentary lifestyle; a diet rich in red and processed meats while being low in fruits and vegetables; smoking and moderate to heavy alcohol consumption.
What are the symptoms of CRC and how is it diagnosed?
Symptoms include changes in bowel patterns (constipation, diarrhea, or fluctuating between diarrhea and constipation), low haemoglobin, blood in the stool, decreased appetite, fatigue, weakness, and unintentional weight loss. However, some individuals show no symptoms at all.
Diagnostic investigations include stool for occult blood and DNA for CRC; a colonoscopy to detect polyps, early and advanced cancer; advanced scans to detect the spread of CRC beyond the colonic wall and serum CEA tests to assess prognosis.
Treatment options include removal of precancerous polyps with endoscopic polypectomy, treatment with endoscopic mucosal resection, surgery, endoscopic stenting, chemotherapy and radiotherapy.
The take home message
Changing dietary habits, the increasing incidence of inflammatory bowel diseases, sedentary lifestyles, smoking and excessive alcohol consumption, and obesity, apart from genetic factors, have resulted in the increasing incidence of CRC all over the world. Early diagnosis, which dictates favourable outcomes and cures for cancer, depends on awareness. Members of the public must consult a doctor if they notice any symptoms – change in bowel habits, rectal bleeding, abdominal pain, unexplained weight loss, fatigue and weakness, feeling of incomplete bowel evacuation, lump or mass in the abdomen, apart from a family history of colon cancer or precancerous polyps, and inflammatory bowel disease. Many international medical organisations have now recommended colonoscopy screening as the only way to detect CRC early, and this is advisable for adults starting at age 45.
Ongoing research on vaccines to reduce the risk of adenoma recurrence, using the gut microbiome to boost anti tumour immunity, and immunotherapy in CRC may bring in more hope to alleviate the sufferings from CRC.
(Prof. Dr. T.S. Chandrasekar is a Padma Shri awardee and senior gastroenterologist with 40 years of experience. He is founder-chairman, MedIndia Hospitals, Chennai. [email protected])
Published – March 20, 2025 03:40 pm IST

