Our skin is the primary victim of sun exposure, and as the summer sun grows harsher each year, protecting it becomes more imperative than ever. For people with vitiligo, a condition marked by depigmented patches of skin, this protection is especially crucial.
Vitiligo is a chronic autoimmune condition that leads to the loss of skin pigment, resulting in patches that are lighter than one’s natural skin tone. Some of the patches may fully turn milky white, and when vitiligo affects areas on the body with hair, the hair in those spots may also turn white or silver. The condition develops when the body’s immune system attacks and destroys melanocytes — the cells responsible for producing melanin, the pigment that gives skin its colour.
Vitiligo cannot be cured, but there are treatments to slow down its progression. The condition doesn’t cause physical pain or pose significant dangers, but it can lead to severe sunburn if the skin is exposed to sunlight without adequate protection. Wearing sunscreen, therefore, is a must.
Moreover, the stigma and shame often associated with vitiligo can create emotional challenges for those living with it.
This International Skin Pigmentation Day on May 25, let’s take a closer look at vitiligo: what causes it, how one can get affected by it, and the ways to treat it.

What are the symptoms?
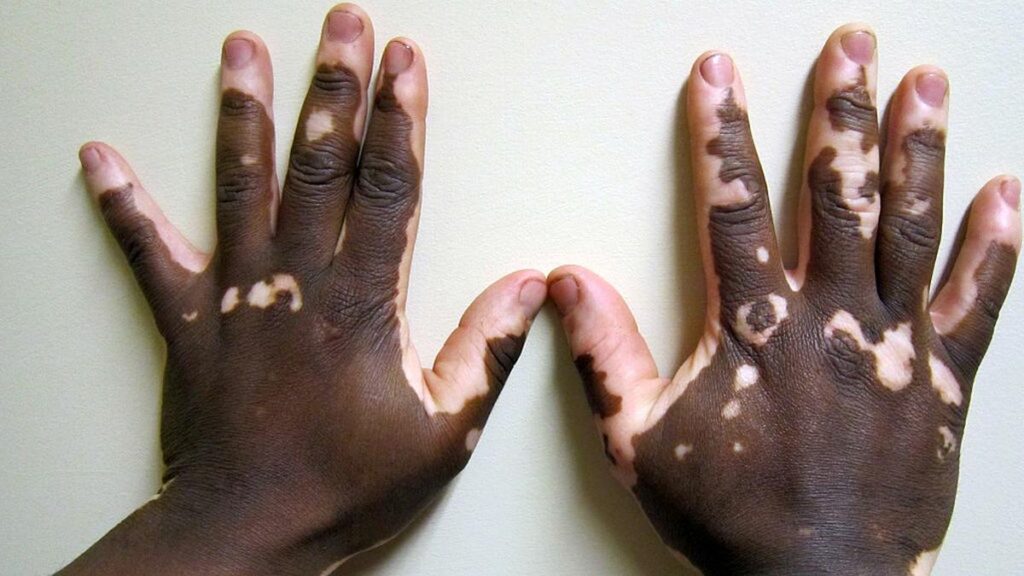
Vitiligo is characterised by depigmented areas of skin. When these areas are smaller than 1 cm, they’re called macules; if they’re larger, they’re called patches.
The condition often begins with a few small white macules or patches that may slowly spread across the body. It commonly first appears on the hands, forearms, feet, and face, but it can also affect any part of the body, including the mucous membranes (such as those in the mouth, nose, genitals, and rectum), as well as the eyes and inner ears.
The extent of pigment loss varies from person to person: some individuals develop only a few small patches, while others experience more widespread depigmentation. Some also experience itchy skin before the depigmentation starts. The symptoms generally start before age 30, but some may also experience it before age 20.
What causes vitiligo and who can get it?
Vitiligo is caused by the lack of melanin in the body. It is an autoimmune condition, which means the body’s immune system mistakes healthy cells — in this case, melanocytes — for harmful invaders like viruses or bacteria. This results in the production of antibodies to destroy the melanocytes.
According to studies, stress or even environmental triggers, like exposure to UV radiation or toxic chemicals, can also play a role in the occurrence of vitiligo.
About 1% of the population experience vitiligo, according to a Pfizer article, and anyone can develop this skin condition, regardless of their gender or colour.
A Cleaveland Clinic article also indicates that about 30% of vitiligo cases are genetic, meaning, they can be inherited from your family members. However, genetic predisposition with respect to vitiligo is more complex as there are multiple simultaneous risk factors at play, according to a 2017 study published in PubMed Central.
Those with certain existing autoimmune conditions, such as Addison’s disease, psoriasis, rheumatoid arthritis, thyroid disease, and type 1 diabetes, are more prone to developing vitiligo, according to a National Institute of Health article.

What are the risks involved?
While vitiligo itself isn’t life-threatening, it can cause one’s skin to be more sensitive to sunlight, and in turn, result in sunburns.
People with vitiligo may also experience slight changes in their eyes, such as abnormalities in the retina or variations in iris colour. In rare cases, inflammation can occur in the retina or iris, though it typically doesn’t affect vision.
Those living with the condition may also have a higher risk of developing other autoimmune disorders, such as hypothyroidism, diabetes, or anaemia.
The mental health challenges posed by vitiligo can be significant. People with the condition may have low self-esteem and tend to avoid social situations. This emotional strain can also contribute to anxiety and depression.
What are the treatment options?
Since vitiligo isn’t curable, treatment options primarily focus on slowing the progression of the condition or enabling repigmentation (restoring the colour of the skin) or depigmentation (removing all colour, ensuring a uniform skin tone).
Medications such as corticosteroids and calcineurin inhibitors may help decelerate depigmentation or even stimulate the regrowth of melanocytes.
Light therapy, which involves directing ultraviolet B (UVB) lights or medical-grade lasers at one’s depigmented skin, helps to restore colour to some extent. Depigmentation therapy, on the other hand, involves the use of monobenzone, a medication applied to the areas of skin that still have pigment.
There are surgical options too, such as using skin grafts from one part of the body to restore or cover affected areas elsewhere. This may, however, not always yield desired results.
Therapy, to deal with the emotional effects of living with vitiligo, is also recommended by healthcare professionals.
Published – May 25, 2025 03:00 pm IST