The landscape of women’s health is constantly evolving and one of the apparent changes has been the major surge in the incidence of cancers in females. The most common cancers diagnosed in females are breast, endometrial (the lining of the uterus) ovarian and cervical cancers. Pathological diagnosis, the cornerstone of accurate diagnosis and treatment is based on histopathologic analysis – the microscopic examination of tissues obtained from tumour samples.
By precisely defining tumour type, grade of the tumour, and extent of invasion, involvement of lymph node etc, histopathologic examination guides critical decisions that impact course of treatment and overall prognosis. However, despite its established role, histopathology faces limitations in early cancer detection, quality variation seen in tissue samples, and limited information for beginning therapy.
The recent years have witnessed a remarkable evolution of newer technological advances fuelled by the use of molecular pathology, liquid biopsies, digital pathology, and other innovative technologies. These transformative technologies have revolutionised our understanding of cancers and paved the way for personalised diagnostics and therapeutics.

Personalised treatment decisions in breast cancer
Breast cancer is the most common cancer among women and the diagnosis of breast cancer is made by analysing core biopsy tissue using radiologic imaging. However, currently this information is not sufficient to plan therapy. This is because all breast cancers are not the same entity and differ in protein expression. Therefore, further testing is very essential to identify the specific molecular type of breast cancer.
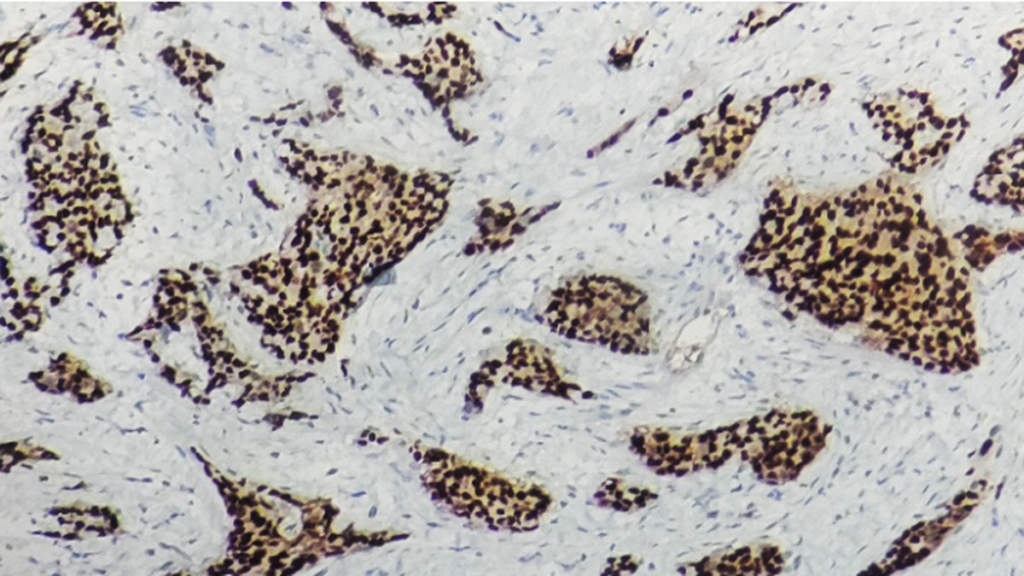
Diagnostic tests known as immunohistochemistry (IHC) help detect the presence of estrogen and progesterone receptors, guiding the use of hormonal therapies such as tamoxifen or aromatase inhibitors. These therapies block hormone signals that stimulate cancer cell growth and aid in killing of cancer cells. Tumour expressing Her 3 Neu receptors (cell surface receptors) will benefit from Herceptin and these tests help in guiding treatment decisions allowing the use of targeted therapies.
If these markers are not expressed, the subtype is termed Triple negative breast cancer type, in which case the patient is not given hormone-based therapy and chemotherapy is administered. This major technological advancement has caused a paradigm shift in treatment and promotes cancer specific therapy.
In addition, advanced molecular based assays also help in predicting disease progression and recurrence. Molecular pathologists perform genomic assays which help determine the risk of recurrence and guide decisions about chemotherapy. For example, in a low-risk breast cancer in a woman with hormone receptor positive may avoid chemotherapy in favour of hormonal therapy.
Women with inherited mutations such as BRCA1 or BRCA2 genes have a significantly higher risk of developing breast cancer. Finding out whether they are carriers is important, so that they can be on close follow up; or be advised to consider prophylactic surgeries (like mastectomy) to reduce cancer risk. Genetic testing helps identify these mutations, and these patients may benefit from PARP inhibitors.

Improved understanding and treatment outcomes in ovarian cancer
Ovarian cancer is often diagnosed at an advanced stage but key advances in pathological testing have significantly helped better understanding and improved patient outcomes. Advanced IHC techniques are used to identify specific markers that help classify ovarian cancer into different subtypes. For example, biomarkers such as WT1, p53, and others are used to differentiate between high-grade serous carcinoma and other subtypes and therapy is designed accordingly.
The use of next-generation sequencing (NGS) and other high-throughput technologies has allowed for deeper genetic analysis of ovarian tumours. This has helped identify specific mutations (BRCA1/BRCA2, TP53, and others) which significantly impact ovarian cancer treatment. New drugs like PARP inhibitors are used in patients with BRCA mutations, improving survival rates by inhibiting the DNA repair in cancer cells.
Cancers are known to produce new blood vessels for their survival and therefore newer treatments targeting blood vessels such as Bevacizumab, are used to inhibit the formation of new blood vessels that tumors need to grow. It is commonly used for advanced ovarian cancer to slow tumour growth and improve survival rates.

Effectively targeting the increasing incidence of endometrial cancer
Endometrial cancer which is the cancer of the uterine lining, has shown increasing trend in the past decade. However pathological techniques have effectively been able to classify the more aggressive tumours from indolent tumours and this has shown promising results with personalised therapy. Treatment is tailored based on molecular classification of endometrial cancer in the biopsy tissue. For hormone receptor-positive endometrial cancers, progesterone therapy can be used as a treatment option, especially for patients who wish to avoid more aggressive treatments like surgery or chemotherapy.
Monitoring high-risk HPV type for cervical cancer
Cervical cancer is often caused by HPV (Human Papillomavirus) infection and HPV DNA testing is used to identify women at risk for cervical cancer. This can effectively guide the decision for surveillance or intervention. Women with high-risk HPV types which can be identified by molecular testing can undergo more frequent screening or be offered prophylactic vaccines like Gardasil.
Specific testing for immunotherapy response
Pathology offers a new testing technique the PDL1 testing which is done on the biopsy tissue to help predict which patients are most likely to respond to immune checkpoint inhibitors, such as pembrolizumab or nivolumab. These drugs help boost the ability of the immune system to fight cancer.

Recent advancements
Liquid Biopsy is an emerging area in cancer diagnostics which can detect genetic mutations and tumour markers from blood samples. This is becoming popular as it is a non-invasive approach and can help in monitoring therapy response and detecting any residual disease after completion of therapy.
Proteomics and metabolomics as diagnostic tools help assess changes in protein expression and metabolic pathways within cancer cells. These insights could lead to new targeted therapies and better biomarkers for early detection and treatment efficacy.
Artificial Intelligence (AI) powered analysis using AI models have demonstrated exceptional accuracy in analysing histopathological images and integrating histologic and molecular data. These models offer deeper insights into tumour types, behaviours, and potential responses to treatment. Advances in AI-driven digital pathology enable the extraction of genomic, transcriptomic, proteomic, and metabolomic biomarkers from routine hematoxylin and eosin (H&E) stained images
Recent technological advancements in diagnostic pathology, including molecular testing, genomics, and immunotherapy targeted testing, are empowering personalised cancer treatment for women with cancers like breast, ovarian, endometrial and cervical cancers. By tailoring treatment to the individual molecular profile, the likelihood of treatment success increases, and side effects may be minimised. Personalised medicine is paving the way for a future where cancer treatment is more precise, effective, and patient centered.
Dr. Sandhya Sundaram is professor, former head and senior consultant, Department of Pathology and Molecular Pathologist, Sri Ramachandra Medical College & Hospital, Chennai. She can be reached at [email protected]
Published – March 26, 2025 06:00 pm IST