The World Health Organization (WHO) records migraine among the top three most common neurological conditions, alongside stroke and dementia, contributing significantly to disability-adjusted life years (DALYs). The Global Burden of Disease (GBD) 2019 study found that headache disorders, including migraines, are a major public health issue, particularly in developing countries like India.
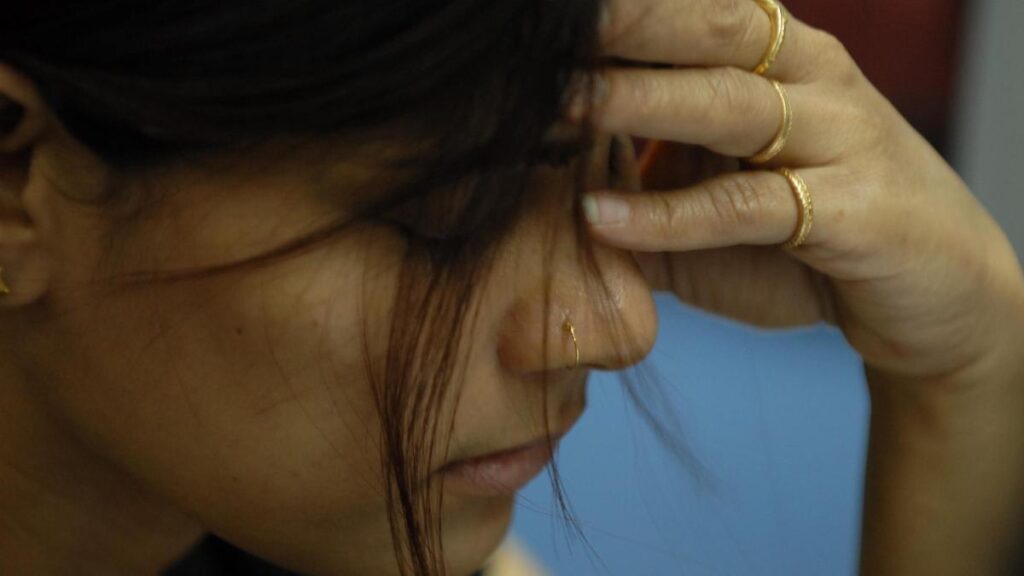
Despite its high prevalence, migraine remains underdiagnosed and undertreated, leading to significant personal, social, and economic burdens.

What is migraine?
Migraine is a headache disorder characterised by recurrent attacks of moderate to severe headaches, often accompanied by nausea, vomiting, and sensitivity to light and sound.
According to the International Classification of Headache Disorders (ICHD-3), migraines can be episodic or chronic and may be preceded by an aura, a series of sensory disturbances, often visual, that can include flashes of light, zigzag lines, or blind spots, and can also involve sensory or language issues.
These headaches typically last between 4 and 72 hours and can significantly impact daily activities. Migraines often begin in puberty and are most prevalent among individuals aged 35–45 years. They are more common in women due to hormonal influences.
The exact cause of migraines remains unknown, but research suggests they result from the activation of pain-producing inflammatory substances around the nerves and blood vessels in the head. Triggers vary from person to person and may include stress, hormonal changes, alcohol, certain foods, lack of sleep, or environmental factors.
What are the signs and symptoms ?
Migraine symptoms vary from person to person, but they generally progress through four stages: prodrome, aura, attack, and postdrome. The prodrome stage, occurring hours or even days before a migraine, includes subtle warning signs like mood changes, food cravings, neck stiffness, frequent yawning, and increased thirst.
The aura stage affects some people and involves visual disturbances like flashing lights, blind spots, zigzag lines, and, in some cases, speech difficulties or tingling sensations in the face or limbs. The attack stage is when the headache begins, usually affecting one side of the head with a throbbing or pulsating pain that worsens with physical activity.
Other symptoms during this stage include nausea, vomiting, and extreme sensitivity to light (photophobia) and sound (phonophobia). The postdrome stage, also called the migraine “hangover,” follows after the headache subsides, leaving individuals feeling drained, confused, or mentally foggy for up to 24 hours.
Beyond these immediate symptoms, migraine poses serious long-term risks. WHO reports that migraine and headache disorders impact work productivity, social interactions, and mental health. Chronic migraine sufferers have a higher risk of developing anxiety and depression due to the frequent disruption of their daily lives.

Who is at risk ?
The GBD 2019 study revealed that India had the highest number of migraine cases in 2019, with over 213 million people affected. Migraines can affect anyone, but certain factors increase the likelihood of developing the condition. Women are more prone to migraines than men due to hormonal fluctuations, particularly during menstruation, pregnancy, and menopause. According to The Journal of Headache and Pain, a family history of migraines significantly raises the risk, suggesting a strong genetic component. Migraines commonly begin in adolescence and peak in middle age, making them especially burdensome for working professionals. Lifestyle and environmental factors such as stress, irregular sleep patterns, dehydration, excessive caffeine or alcohol consumption, and dietary triggers can contribute to migraine attacks.
Additionally, healthcare costs related to migraines, including doctor visits, medications, and hospitalisations, place a heavy strain on healthcare systems worldwide. Despite these risks, many individuals do not receive proper diagnosis and treatment, leading to prolonged suffering and reduced quality of life.
What are the treatment options?
It is crucial to seek professional medical advice rather than completely rely on over-the-counter pain relievers for a long period, which may provide temporary relief but could worsen the condition in the long run.
Healthcare professionals may recommend preventive treatments for those with frequent or severe migraines. These may include medications such as beta-blockers, antidepressants, or anti-seizure drugs, prescribed based on an individual’s medical history.
According to an article in The Lancet, in recent years, calcitonin gene-related peptide (CGRP) inhibitors have emerged as an effective option for managing chronic migraines, but they should only be used under medical supervision.
Non-medical strategies also play a vital role in reducing migraine frequency. Maintaining a consistent sleep schedule, staying hydrated, managing stress through relaxation techniques, and avoiding known triggers can help prevent attacks. Many individuals benefit from lifestyle modifications, behavioural therapy, and structured migraine management plans designed by healthcare providers.
Despite the availability of treatments, WHO reports that millions of people with migraines do not receive proper diagnosis and care, particularly in low-income regions. Public health efforts focus on increasing awareness, improving healthcare access, and reducing the stigma around migraines to ensure that more people receive the treatment they need. If you experience frequent or severe headaches, consult a qualified healthcare professional for an accurate diagnosis and personalised treatment plan.
Published – March 20, 2025 02:22 pm IST