
The current study highlights that any timely treatment to restore blood flow is lifesaving, even if limited to fibrinolysis.
Can telemedicine guidance on a messaging platform like WhatsApp help doctors improve treatment outcomes in patients presenting with major heart attacks? The Tamil Nadu Government Heart Attack Management Programme – operationalised in a hub-and-spoke model networking 18 government medical college hospitals and 188 district/taluk government hospitals – has the answer.
A study analysing the five-year experience (2019-2023) of the programme has found that it has demonstrated that WhatsApp groups are a cost-effective way of networking larger and smaller hospitals in a hub-and-spoke model to provide telemedicine guidance for early diagnosis and treatment of major heart attacks (STEMI-ST-segment elevation myocardial infarction). Through this, cardiologists in larger hub hospitals offered telemedicine guidance to smaller spoke units. Additionally, these groups were used to coordinate patient transfers between hospitals and to monitor the entire process.
Putting out the key findings in an article published recently in the Indian Journal of Medical Research – ‘Impact of telemedicine in STEMI care system: A five-year experience from Tamil Nadu, India’ – government cardiologists and health officials reported that that the government-sponsored STEMI care system in a hub-and-spoke model, guided by telemedicine via WhatsApp groups, significantly improved guideline-directed treatment for STEMI care in a resource-limited setting.

How the programme was implemented
Talking about the implementation of the initiative, G. Justin Paul, professor of cardiology, Madras Medical College, and the programme’s nodal officer, explained that the 18 government medical college hospitals in T.N. were equipped with cardiac catheterisation laboratories to offer Percutaneous Coronary Interventions (PCI), thereby serving as hub hospitals. Additionally, 188 district and taluk-level government hospitals lacking PCI capacity were enabled to administer clot busting medicines and were linked to these 18 hubs as spoke hospitals. Eighteen STEMI clusters were established by networking 10-15 spoke hospitals with each hub based on geographical proximity and transport logistics.
The networking was done in two phases – 12 hubs linked to 154 spokes to form 12 clusters in phase I (2017-2018) and six hubs linked to 34 spokes to create six more clusters in phase II (2019-2020).
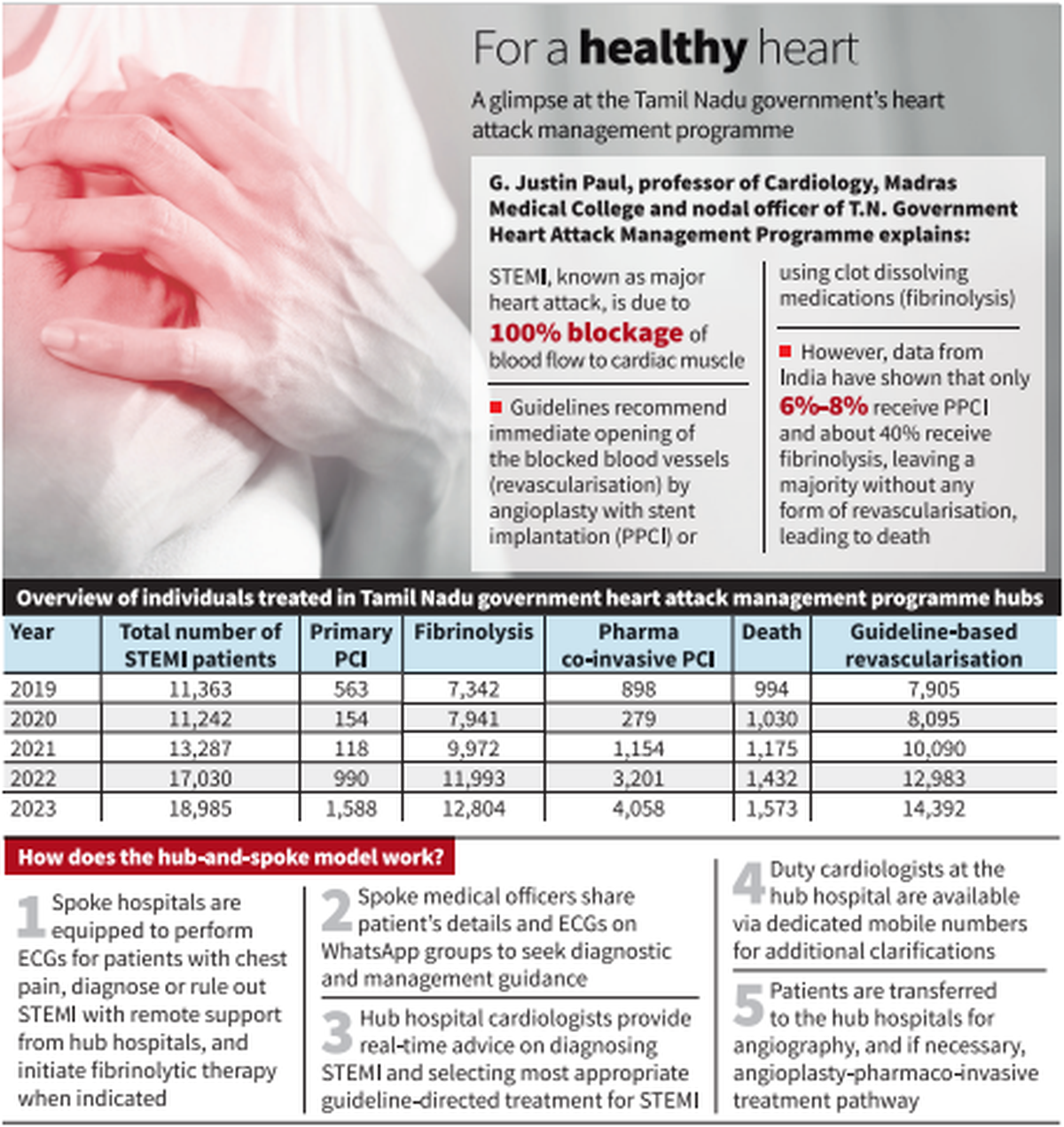
The authors noted that 18 WhatsApp groups – one for each cluster – were created to facilitate case-specific management of persons with suspected heart attacks. These groups enabled seamless communication between cardiologists at hub hospitals and teams at spoke hospitals.

The results
In total, 71,907 individuals with STEMI were treated over the five years. There was a 67% annual increase in the total number of individuals treated for STEMI. The proportion of individuals receiving pharmaco-invasive therapy increased from 7.9 to 31.7%. There was a 68% increase in the number of individuals receiving primary PCI. The number of individuals who did not receive guideline-directed treatment decreased by 20%.
The analysis found that there was a 6.7-fold rise in the individuals referred from spoke to hub hospitals for catheter-based revascularisation. The overall mortality showed a marginal decrease from 8.7 to 8.3%; phase-II hubs achieved a 68% reduction from 8.5% to 5.8% aligning with a rise in guideline-directed treatment.
Dr. Paul said that in developed nations, STEMI care was centred on timely primary PCI, which must be done within 90-120 minutes by a specialist team in a cath lab. But this set up requiring 24×7 infrastructure and trained interventional cardiologists was not feasible in many developing nations including India.
“The current study highlights that any timely treatment to restore blood flow is lifesaving, even if limited to fibrinolysis. Any form of revascularisation is definitely better than no revascularisation at all. Healthcare systems in developing nations must focus on early heart attack and at least start with fibrinolysis. This forms the foundation in which a pharmaco-invasive system can be built, as healthcare capabilities expand,” he added.
Published – April 10, 2025 08:32 pm IST

