“A disease is not cured by merely repeating the name of the medicine. It requires direct realisation” : Vivekachudamani
Donald Schon, an American philosopher, who developed the concept of reflective practice said that professional growth begins when an experience is viewed through a critical lens. A critical reflection is one that contemplates with evaluation, balances reasoning and develops future options and plans.
Healthcare involves a complex interaction (human factors) between people: person and environment and person and machines. These interpersonal interactions involve not only the doctor-patient relationship but also interprofessional dynamics including administrative challenges. Dynamic decision making associated with these complex interactions can result in significant medical errors and adverse patient outcomes.
Simulation has been used successfully in many fields to assess and to create models. In medicine, a field that involves high stakes, simulation was introduced relatively late, by David M. Gaba, who built the first patient simulator in 1986. He describes simulation as a technique and not a technology. The technique was to deliver real-world problems as guided experiences. This experience is followed by a facilitated reflection.
Simulation in medical education
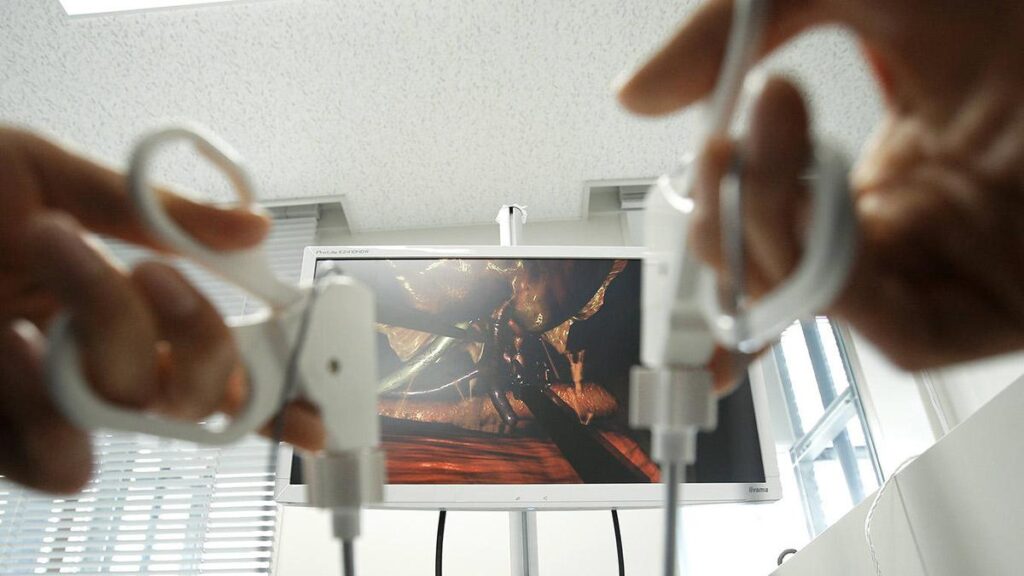
Simulation-based medical education can be delivered either in a lab, in-situ (at the actual place of work) or even in the community. The various modalities involved include mannikin-based simulation, screen-based, model-based, simulated participant or the use of virtual or augmented reality.
The National Medical Commission aims to produce an Indian Medical Graduate with essential skills involving leadership, communication and lifelong learning rather than mere clinical practice. The traditional method of teaching in medical colleges involves lectures, observation and assisting, followed by a learning curve largely relying on a “role model theory”.
The future of healthcare depends on providing evidence-based training on these aspects including training for our future educational leaders. Challenges with the traditional approach include decreased flexibility and innovation and the presence of a passive learning environment, which is more apparent with the increasing number of seats. The quality of graduates varies widely among colleges due to differences in resources – financial, faculty, patients, as well as physical infrastructure.
The current generation is a cohort of adaptable learners with self-directed learning and an increasing sense for social learning. Generation Z and Generation Alpha, growing up in a digital-first world, are naturally inclined toward technology-driven learning methods, making simulation an ideal approach for medical education in India. These learners are quick to adapt to interactive tools like virtual reality, augmented reality, and gamified simulations, which enhance engagement and knowledge retention. Traditional lecture-based methods may not resonate as effectively with the tech-savvy generations. By incorporating simulation techniques into medical curricula, we can align education with the learning preferences of newer generations.

Simulating real-life medical scenarios
Simulation can be likened to the Indian concept of maya—an illusion that mirrors reality, allowing learners to experience clinical situations without real-world consequences. Just as maya creates a convincing, yet controlled environment, simulation presents lifelike scenarios where students can act, reflect, and learn.
The actions taken during simulation shape future clinical behaviour, by reinforcing good practices and correcting errors. This reflective learning helps build confidence, decision-making skills, and emotional readiness. For Indian medical students, especially in varied healthcare settings, simulation offers a safe space to prepare for real-life challenges, where each simulated experience influences future patient care.
This approach not only improves clinical competence but also fosters innovation, critical thinking, and a deeper understanding of patient care. With the availability of information at the fingertips, the need is to facilitate the application of knowledge, reflect on it and to contextualise the information.
Simulation for medical education aligns with key educational philosophies like constructivism, positivism, and pragmatism. Constructivism emphasises learning through experience, where students build knowledge by engaging in realistic clinical scenarios. Positivism supports the idea of objective learning through measurable outcomes—simulation provides data on performance, helping assess skills accurately. Pragmatism focuses on practical, real-world application of knowledge, which simulation naturally supports by bridging theory and practice. Together, these philosophies validate simulation as a comprehensive teaching method, enabling Indian medical learners to gain hands-on experience, develop critical thinking, and translate academic knowledge into effective, context-based clinical practice.
There is enough evidence for delivery of technical and non-technical skills through simulation. For example: training in communication with a patient who is aggressive, mass casualty, health education, pandemic training and maternity care. COVID-19 was a powerful example of how simulation can play a crucial role in medical education, particularly in a country like India. During the pandemic, the need for rapid upskilling of healthcare professionals became urgent, and traditional training methods were severely disrupted. Simulation-based education emerged as an effective alternative, allowing medical students, nurses, and doctors to practice clinical skills, emergency response, and patient management in safe, controlled environments. The pandemic highlighted the importance of integrating simulation into the core medical curriculum to build competence and confidence.
Decentralising education
Simulation-based training for students, when in rural areas, holds immense potential for transforming medical education in India. Rural healthcare facilities often face shortages of trained professionals, limited clinical exposure, and inadequate infrastructure, making it difficult to ensure consistent, high-quality medical training. Simulation offers a practical solution by providing hands-on, experiential learning without relying on real-time patient availability. Mobile simulation labs, low-cost manikins, and virtual reality platforms can bring standardised training to even the most remote regions. These tools allow rural medical students and healthcare workers to practice essential clinical skills, such as basic life support, trauma care, and maternal-child health interventions, in a controlled and repeatable environment.
By decentralising education and making it more accessible, simulation can bridge the urban-rural healthcare gap and empower local providers to deliver safer, more effective care. Furthermore, as India continues to invest in its healthcare infrastructure, integrating simulation into rural medical colleges and training centres will be key to building a more resilient and equitable health system. With the right support and innovation, simulation-based training can become a cornerstone in shaping competent, confident healthcare professionals across India’s rural landscape.

Simulation in medical education has a transformative impact at multiple levels—global, national, organisational, and individual. At the global level, simulation promotes standardised training, enhances patient safety, and reduces the incidence of medical errors, contributing to more consistent healthcare outcomes across countries. Simulation can in itself be used for quality assessments and improvements.
For healthcare organisations and medical institutions, simulation improves training efficiency, reduces risks during live procedures, and enhances team communication and crisis management. This leads to better clinical outcomes, reduced patient harm, and increased trust in healthcare services. At the individual level, simulation builds confidence, sharpens technical and decision-making skills, and fosters reflective learning. Students and professionals can practice repeatedly in a safe environment, learning from mistakes without consequences.

AI, virtual reality and more in medical simulation
The use of virtual reality (VR) in simulation for medical education in India is revolutionising how students and professionals learn clinical skills. VR creates an immersive, interactive environments where learners can practice surgeries, anatomy, and emergency scenarios without risking patient safety. It is especially valuable in India, where clinical exposure can be inconsistent due to overcrowded hospitals and resource limitations. With VR, students gain standardised, repeatable experiences that enhance understanding and confidence. As the technology becomes more affordable, integrating VR into medical curricula across India can bridge training gaps, improve skill retention, and prepare future healthcare providers for real-world challenges more effectively.
Simulation plays a vital role in addressing serious adverse events by allowing learners to experience and manage critical scenarios without harming real patients. Through realistic simulations of medical errors, complications, or emergencies, students and professionals can practice recognising warning signs, making swift decisions, and coordinating effectively with teams. This hands-on approach enhances clinical judgment, reduces anxiety, and improves patient safety outcomes. In India, where varying healthcare settings may limit exposure to high-risk cases, simulation ensures all trainees are better prepared. By integrating such training, medical institutions can foster a culture of safety and accountability in healthcare.
Challenges in using simulation
Assessment plays a major role in competency-based education. The current assessment methods do not allow for assessment of the skill of critical reflection. One of the challenges in the use of simulation for assessment is that a good performance in a simulation does not guarantee a good real-life performance and vice versa. By embedding simulation into medical education across India, the country can create a more competent, confident, and future-ready healthcare workforce—one that benefits not only the nation but contributes meaningfully to global health advancement.
The NMC has issued guidelines on the use of simulation for medical colleges including the requirements of space and other resources. One of the major challenges for the colleges has been the cost of the simulators, training faculty and for setting up the lab. While faculty training can be addressed, the resource availability depends on the financial health of the institute and buy-in of stakeholders – both governmental and private. To overcome this barrier, we need economic evaluation of education including both direct and indirect outcomes. Educational investments can increase only by demonstrating the cost-benefit of such ventures.
The other challenge in incorporating simulation, comes from the faculty with the idea that a simulator can never be a substitute for a real patient. This must be analysed from various perspectives. The patient is usually unaware of the experience of the doctor, and it can be considered unethical to start learning “on the patient” rather than to be trained in a simulated environment before involvement in actual care. From the student’s perspective, a simulated environment can provide necessary confidence and allow them to analyse the situation. Simulation can also help in addressing the challenge of the absence of a protected time for learning especially for postgraduate education.
In postgraduate education, the balance of clinical work with that of education is a constant battle. In situ simulation can help include hospital processes providing reflection and analysis of real-life decision making. By providing a psychologically safe environment for learning and a necessary pause, this method can also address burn-out among the students. But psychological safety should be balanced with realism, as it carries a risk of translation of behaviour in a simulated environment to the real world – for example, the need to include patient death because of incorrect action during simulation.

The future of simulation
Simulation-based education helps a student encounter and address various processes present in healthcare – for example interprofessional interaction, conflicts arising in the workplace, decreasing waiting times for the patient, which are not a part of the curriculum but make an impact in the real world.
Simulations are seen as too objective with a lot of unknown or “black box” factors. Education is a behavior and is non-linear and difficult to quantify. So, we risk making a McNamara fallacy – measuring all that is measurable, disregarding the unmeasurable, not giving importance to the unmeasurable, and considering the unmeasurable non-existent. But there is a constant need to study how to accurately represent phenomena in a simulated world with a single intention of having a learning – both intended and unintended out of it.
What is the future of simulation-based education in healthcare? This includes its use of standardised scenarios for assessment, regular training, remote location training, use of artificial intelligence and analytics to improve reflection.
Simulation is not a “solve all” in medical education but will go a long way in bringing relevance to the medical education in the current era of information overload.
(Dr. Balaji Singh is Dean, Sri Ramachandra Medical College, Chennai. [email protected]; Dr. Sree Kumar E J is Associate Professor, Department of Anaesthesiology and Fellowship in Healthcare Simulation [email protected])
Published – April 30, 2025 03:29 pm IST