While the general prevalence of systemic lupus erythematosus (SLE) in India is reported as 3.2 per 100,000 population, specific data on various types of lupus within India are limited. Studies on SLE in India have primarily focused on the overall disease prevalence and its clinical features.
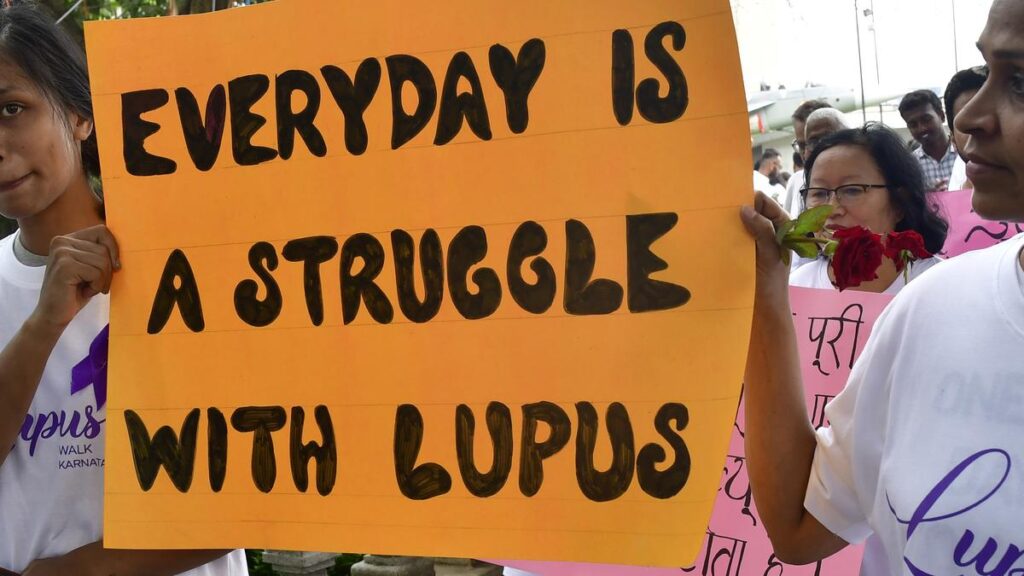
According to studies, lupus care in India faces challenges related to access, cost and awareness. Specifically, limited access to specialised rheumatologists, financial burdens, and inadequate insurance coverage contribute to difficulties in diagnosis and management. Furthermore, stigmas associated with chronic illnesses and lack of awareness among healthcare providers and the public can lead to delays in seeking medical help.
What is lupus?
Lupus is a long-term, progressive autoimmune disease in which the immune system mistakenly attacks healthy tissue throughout the body.
According to the Centers for Disease Control and Prevention (CDC), lupus can affect any part of the body, including the skin, joints, kidneys, lungs, heart, and brain. The World Health Organization (WHO) notes that lupus involves chronic stimulation of the immune system, and its exact cause remains unknown. The Lancetdescribes lupus as a multisystemic autoimmune disease marked by the presence of autoantibodies against nuclear antigens, immune complex deposition, and chronic inflammation — primarily affecting classic target organs like the skin, joints, and kidneys
Lupus, has several forms, with Systemic Lupus Erythematosus (SLE) being the most common and serious type. Other forms include Cutaneous Lupus Erythematosus (CLE), which primarily affects the skin. Within CLE, there are further subtypes like Discoid Lupus Erythematosus (DLE), which is characterised by circular lesions, and Subacute Cutaneous Lupus Erythematosus (SCLE), which often presents with rashes and joint pain. Drug-induced lupus can occur as a side effect of certain medications, while neonatal lupus affects newborns.
What are the signs and symptoms ?
Signs and symptoms of lupus can be wide-ranging and unpredictable.
It is a highly variable disease. This means that the symptoms, their severity, and the way the disease progresses can differ significantly from person to person — with some experiencing mild symptoms and others facing life-threatening complications.
The most common symptom, as reported by the CDC, is extreme fatigue, which can significantly impact both physical and mental well-being. Other frequent symptoms include pain or swelling in the joints and muscles, fevers, hair loss, frequent mouth sores, and a characteristic butterfly-shaped rash across the cheeks and nose.
Less common but important symptoms may involve chest pain during deep breathing, heightened sensitivity to sunlight, cognitive and mental health changes, damage to the eyes, and complications in vital organs such as the heart, lungs, and kidneys.
The WHO emphasises that the variation in affected organs may reflect different underlying immune pathways, supported by distinct autoantibody profiles. These symptoms tend to occur in episodes, known as flares, which can be followed by periods of remission where symptoms temporarily subside.

Who is at risk?
Anyone can be at risk of being affected by lupus. However, certain populations are more vulnerable. The CDC and a report in Nature highlight that it primarily occurs among women between puberty and menopause and is more common among individuals of African American, Hispanic, Asian, and Indigenous descent. While its can occur at any age, it’s most often diagnosed between 15 and 45 years old. It affects approximately 3.4 million people worldwide, with 400,000 individuals being newly diagnosed each year
Though the exact cause remains unknown, WHO suggests that genetic predisposition combined with hormonal and environmental triggers likely contributes to disease development. Studies also indicate that the chance of developing SLE is believed to be associated with genetic factors, epigenetic factors , environmental triggers, and hormonal factors. Differences in clinical patterns among patients suggest that multiple disease mechanisms may be involved, making the condition highly individualised.
What are the treatment options?
Treatment for lupus aims to manage symptoms, prevent organ damage, and maintain low disease activity or achieve remission.
The Lancet outlines current therapeutic approaches –under personalised guidance from heathcare professionals — starting with hydroxychloroquine as a baseline medication, often supplemented with corticosteroids and immunosuppressants depending on severity.
In recent years, newer therapies like belimumab, anifrolumab, and voclosporin have been approved, particularly improving outcomes for patients with lupus nephritis — a kidney disease caused by SLE. Alongside medications, non-pharmacological strategies are essential, including lifestyle interventions, sun protection, mental health support, and patient education to improve quality of life and treatment adherence.
The WHO points out that despite medical advances, there is still no universally reliable marker for diagnosis or disease activity, and access to newer treatments remains unequal globally. The primary goals of treatment are to suppress immune overactivity, manage flares, and reduce long-term complications such as infections, osteoporosis, and cardiovascular disease caused both by the illness and its treatments.
Published – May 10, 2025 11:50 am IST