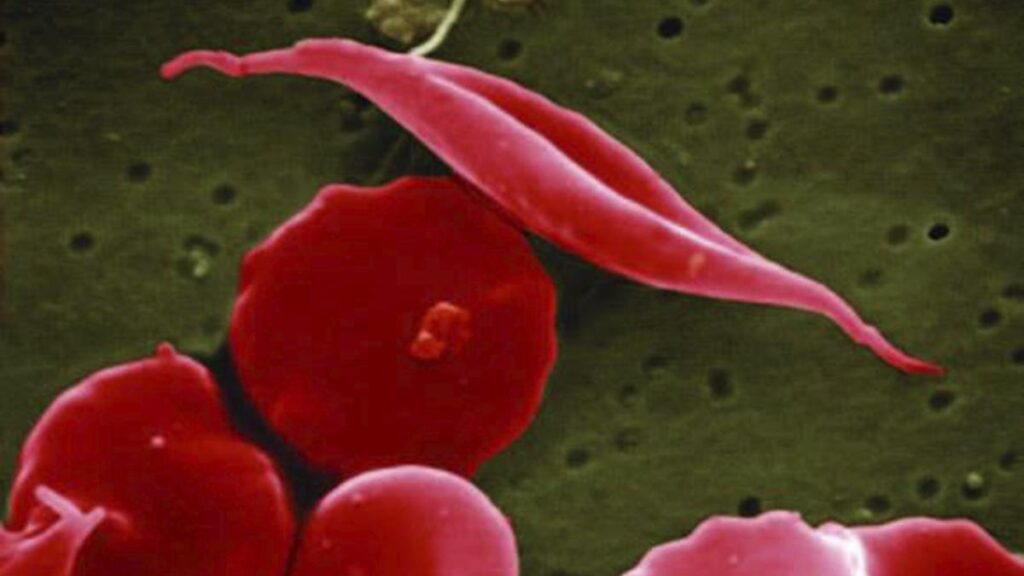
This electron microscope image provided by the National Institutes of Health in 2016 shows a blood cell altered by sickle cell disease, top. (National Center for Advancing Translational Sciences (NCATS), National Institutes of Health via AP). File photograph
| Photo Credit: AP
It’s a disease that not many know about, despite estimates indicating that India carries the second-highest burden globally. Sickle cell disease, a group of inherited blood disorders, affects around 1 million people in India, a significant proportion of whom are concentrated in tribal belts across Odisha, Jharkhand, Chhattisgarh, Madhya Pradesh, and Maharashtra.
June 19 is observed as World Sickle Cell Awareness Day and this year’s theme is: ‘Global Action, Local Impact: Empowering Communities for Effective Self-Advocacy.’ Here is all you need to know about sickle cell disease.
What is sickle cell disease?
Sickle cell disease refers to a group of inherited blood disorders. A genetic mutation causes the body to produce abnormal haemoglobin. Haemoglobin is a protein containing iron, found in the body’s red blood cells. It plays a crucial role in transporting oxygen from the lungs to the rest of the body. In patients with sickle cell disease, the abnormal haemoglobin causes the shape of the red blood cells to change. Healthy red blood cells are round, and can easily move throughout the body, delivering oxygen. In sickle cell disease, the red blood cells are shaped like a sickle (hence the name) or a crescent, and become rigid and sticky. The sickle cells can slow or block blood flow, hampering the delivery of oxygen to organs and tissues, causing pain and other complications. In addition, sickle red blood cells are more fragile than normal red blood cells: they last only 10 to 20 days as opposed to 90 to 120 days that the normal red blood cells last, which means the body may have a lower number of red blood cells — anaemia.

How does it occur?
Sickle cell disease is inherited. When both parents have a copy of the sickle cell gene and the child inherits both copies, then the child gets sickle cell disease. If the child inherits only one copy of the sickle cell gene, the child has sickle cell trait — this means that there is one normal haemoglobin gene and one sickle cell gene. These children generally do not have symptoms, but are carriers, and can pass on the gene to their children.
Sickle cell disease is an umbrella term; sickle cell anaemia refers to a type of sickle cell disease, a common and severe form.
A 2024 analysis, ‘Prevalence of Sickle cell disease, Sickle cell trait and HBS-beta-thalassemia in India: A systematic review and Meta-analysis’ by Priyanka Rao et al, estimated the prevalence of sickle cell disease (SCD) and sickle cell trait (SCT) to be 1.17% and 5.9% in India. Madhya Pradesh, Chhattisgarh, and Maharashtra have a high prevalence of SCD and SCT, with the burden relatively higher among the tribal communities, the analysis said.
What are the signs and symptoms?
Signs of sickle cell disease usually manifest from early childhood. Signs and symptoms vary from person to person and may range from mild to serious. Some symptoms include: anaemia, which can cause tiredness and shortness of breath and weakness; periodic episodes of pain, known as pain crises, which occur when blood flow is blocked, often to the chest arms of legs; swelling of hands and feet caused by blocked blood circulation; yellowing of the skin and eyes (jaundice); delayed growth and a frequent infections.
What are the complications of sickle cell disease?
There are a number of complications that can arise with this disease. These include: acute chest syndrome, which occurs when oxygen flow to the lungs is blocked and can be a medical emergency; stroke, when there is an interruption to blood flow to the brain; splenic sequestration or splenic pooling, when sickle cells get stuck in the spleen, causing it to enlarge and leading to a sudden drop in the number of circulating red blood cells and priapism, when sickle cells block blood vessels in the penis causing pain and potentially permanent damage.

How is sickle cell disease treated?
Treatment of sickle cell disease usually involves the management of symptoms and the prevention of complications.
A bone marrow (stem cells transplant) can cure the disease. This involves replacing the bone marrow of the patient with bone marrow from a healthy, genetically matched donor. However there are risks involved, the procedure may not be suitable for all, and it is expensive.
Other treatments involve the use of medications to help lessen pain crises, lower the risk of anaemia and improve blood flow. One significant drug used in treatment is hydroxyurea. Pain relieving medications may also be prescribed. Some patients may require blood transfusions to increase the number of healthy red blood cells in their body and prevent symptoms and complications. Antibiotics may be prescribed to prevent infections.
Recently, gene editing therapy for sickle cell disease has become possible. In December 2023, the United States’ Food and Drug Administration (FDA) approved of two treatments: Casgevy and Lyfgenia, “representing the first cell-based gene therapies for the treatment of sickle cell disease (SCD) in patients 12 years and older. Additionally, one of these therapies, Casgevy, is the first FDA-approved treatment to utilise a type of novel genome editing technology, signaling an innovative advancement in the field of gene therapy,” as per its website. In May 2024, a 12-year-boy in the U.S. became the world’s first patient to receive gene therapy, which involved the removal of his bone marrow cells, their genetic tweaking and then their replacement in his body.

What is India’s response to the sickle cell challenge?
In 2023, the Centre launched the National Sickle Cell Anaemia Elimination Mission to eliminate sickle cell disease as a public health problem by 2047. The overall aim of the mission, as per its website, is to enable access to affordable and quality health care to all SCD patients, and to lower the prevalence through awareness, change of practices and screening interventions. The initial focus is to be on 17 high prevalence States. However access to drugs and treatment continue to remain major challenges for a large number of patients in India.
Published – June 19, 2025 07:00 am IST