There is a correlation between stress and stroke. A recent study published in Neurology, the medical journal of the American Academy of Neurology, suggests that people experiencing chronic stress may have a higher risk of stroke. A Lancet study analysed data from the Global Burden of Disease Study (GBD) 2021, highlighting a significant increase in stroke cases from 1990 to 2021, with various contributing risk factors, including stress, on the rise.
The study shows that approximately 12 million new strokes occur each year, and one in four people above 25 years will have a stroke in their lifetime. Furthermore, almost 94 million people globally are living with the after-effects of stroke.
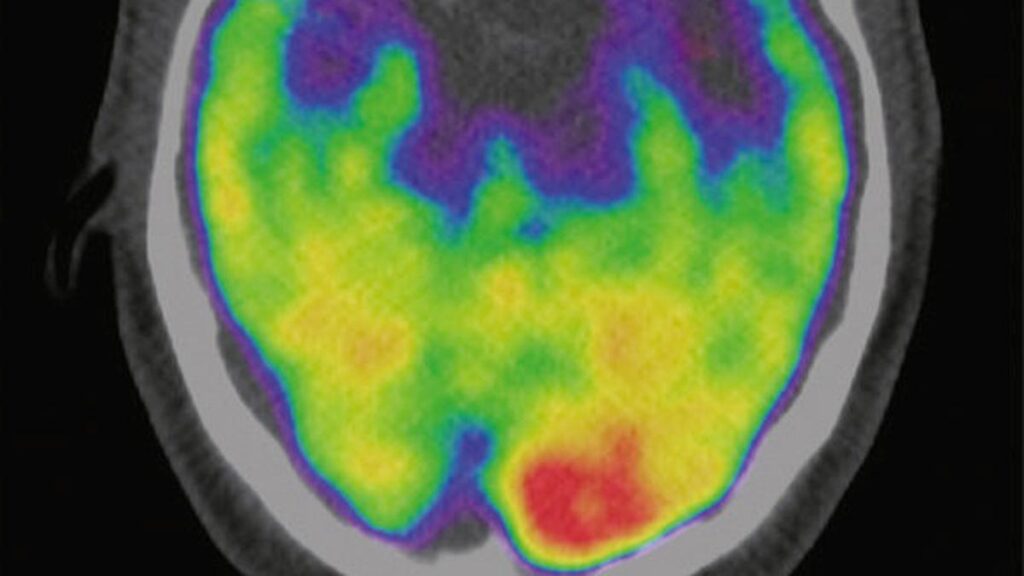
Chronic stress can lead to hypertension, a major risk factor for ischemic strokes, caused by blocked blood vessels, and hemorrhagic strokes caused by bleeding in the brain due to a ruptured blood vessel. Also, stress often contributes to unhealthy lifestyle choices, such as increased consumption of alcohol, smoking, poor diet, and lack of exercise, which further elevate stroke risk.

The link between stress and strokes
S. Karthikeyan, senior consultant, interventional neurologist at Apollo Hospitals, Chennai, acknowledges that while stress and strokes may not always have a direct link, extreme stress can elevate the risk. “There are studies, as well as my own clinical experience, that indicate stress can be a potential stroke trigger,” he says.
According to the World Stroke Organization (WSO), mental health plays a significant role in stroke risk, and around one in six strokes is linked to depression and stress. Prabash Prabhakaran, head and senior consultant, neurology, at Apollo Speciality Hospitals, Chennai, points out how stress often indirectly increases the risk of strokes by affecting multiple physiological factors.
“Stress exacerbates risk factors like hypertension, diabetes, and high cholesterol, which can eventually lead to a stroke,” he says.
According to Nasiruddin G, consultant, internal medicine at Fortis Hospital, Bengaluru, stress-related hormonal changes increase blood pressure, disturb sleep, and raise cholesterol levels, further impacting heart health and brain function.

A combined risk across all age groups
The WSO highlights that people struggling with various mental illnesses are almost two times at greater risk of stroke and Transient Ischemic Attacks (TIA), or “mini-strokes“, a temporary disruption of blood flow to the brain, particularly in adults who are middle-aged and older. The GBD study finds that 53% of strokes occur in people below 70 years. And 53% of strokes occur in men, while 47% occur in women. Notably, 22% of people living with stroke are between 15-49 years old.
Addressing this, Dr. Prabhakarn emphasises that a stroke can affect any age group, even though it is more common after 45. “Stress is an add-on threat that will increase the risk in any age group; this is why there should be clinical evaluations of one’s mental health. While treating stroke cases, there needs to be an overall treatment plan to address this,” he says. Adding to this, lifestyle changes in various age groups due to stress, such as unhealthy eating, alcohol consumption, smoking, and lack of exercise, can also contribute to stroke. “Stress can cause chronic inflammation in the body in whatever age group you are, which can increase the risk of stroke,“ says Dr. Nasiruddin.
The GBD study shows a crucial finding: stroke is highly preventable. In 2021, a staggering 84% of the global stroke burden was attributed to 23 modifiable risk factors. This means that by addressing these risk factors, individuals and communities can significantly reduce their risk of stroke.

Post-stroke rehabilitation gaps
According to Dr. Prabhakaran, one of the overlooked aspects of stroke management in India is post-stroke rehabilitation. “While awareness about stroke is better now, we need to focus on rehabilitation services. The government can help make rehabilitation more accessible and affordable for all,” he says. He points out that post-stroke depression (PSD) is a major challenge, as many stroke survivors struggle with psychological distress especially due to stroke-induced mobility loss. Dr. Prabhakaran also stresses that rehabilitation services are largely confined to tertiary care hospitals in urban areas, making them inaccessible to many stroke survivors in rural regions.
A study published in Frontiers in Neurology and Neuroscience Research found that the prevalence of PSD among Indian stroke survivors ranges from 24% to 90%, with an overall prevalence of 55%.
Additionally, out-of-pocket healthcare costs limit access to psychiatric and neurorehabilitation services and invariably add to the stress of the patient. Dr. Prabhakaran says that the lack of integrated care models further worsens the issue, as psychiatric rehabilitation is often disconnected from stroke rehabilitation programmes.
“Stroke patients reach a 40-50% recovery post-treatment, but a full recovery requires effective rehabilitation. Unfortunately, rehab is often considered a luxury in India due to out-of-pocket expenses,” he says. He says while many parts of India have advanced stroke care facilities, there is still a gap in accessible and affordable neurorehabilitation services.

Government and follow-up care
Experts say that alongside personalised care in treating stroke, there needs to be government intervention in the care that follows, making post-stroke rehabilitation the need of the hour.
According to the experts, stroke survivors face significant physical and mental challenges as they navigate life after a stroke. To ensure the best possible outcomes and prevent future stroke episodes, experts emphasise the importance of a comprehensive treatment plan guided by a multidisciplinary team of specialists. “Stroke survivors require a coordinated approach to care,” says Dr. Karthikeyan.
Talking about personalised care for stroke survivors, Dr. Prabhakaran says that a team of specialists, including neurologists, physicians, psychologists, and other departments as needed, should work together to develop a personalised treatment plan that addresses patients’ needs.
According to Preetha P., consultant neurologist at Prashanth Hospital, Kolathur, Chennai, addressing the cost barriers in post-stroke rehabilitation care is vital. “While treatment plans often include essential therapies like speech therapy and physiotherapy, affordability and accessibility remain significant challenges, limiting their reach to all those in need,” she says.
To bridge this gap, experts say that existing rehabilitation facilities need to be strengthened with more government intervention.
Published – June 04, 2025 07:00 am IST