On New Year’s Day, five-year-old Mayuri lost her life to a snakebite in Uttara Kannada district in Karnataka. The delay in receiving antivenom and the unsafe conditions at her anganwadi tragically sealed her fate. She became one of the estimated 58,000 Indians who die every year from venomous snakebite, a terrible number that renders India the ‘snakebite capital’ of the world and highlights the scale of this preventable crisis. What makes snake venom so deadly, and how does antivenom neutralise its effects?
What are antivenoms?
Antivenoms, or antivenins, are life-saving medicines used to treat snakebites. They are produced by injecting small amounts of venom into animals, usually horses, which then produce antibodies as part of their immune response. These antibodies become antivenoms.
Snake venom is one of nature’s most lethal weapons, a complex cocktail of toxic proteins, each tailored by evolution to immobilise, and in some cases to digest, prey and defend against threats. When a sufficient quantity of venom is injected during a snakebite, the toxins wreak havoc on the human body in multiple ways. Haemotoxins destroy blood cells and disrupt clotting. Neurotoxins block nerve signals and paralyse. Cytotoxins dissolve tissue at the bite site. The effects are often fatal without medical intervention.
Antivenoms are the frontline defence. They work by specifically binding to the venom toxins to render them ineffective, allowing the body’s natural defence systems to clear them safely over time. But for antivenom treatment to succeed, responders need to know which snake species inflicted the wound and how much venom it injected.
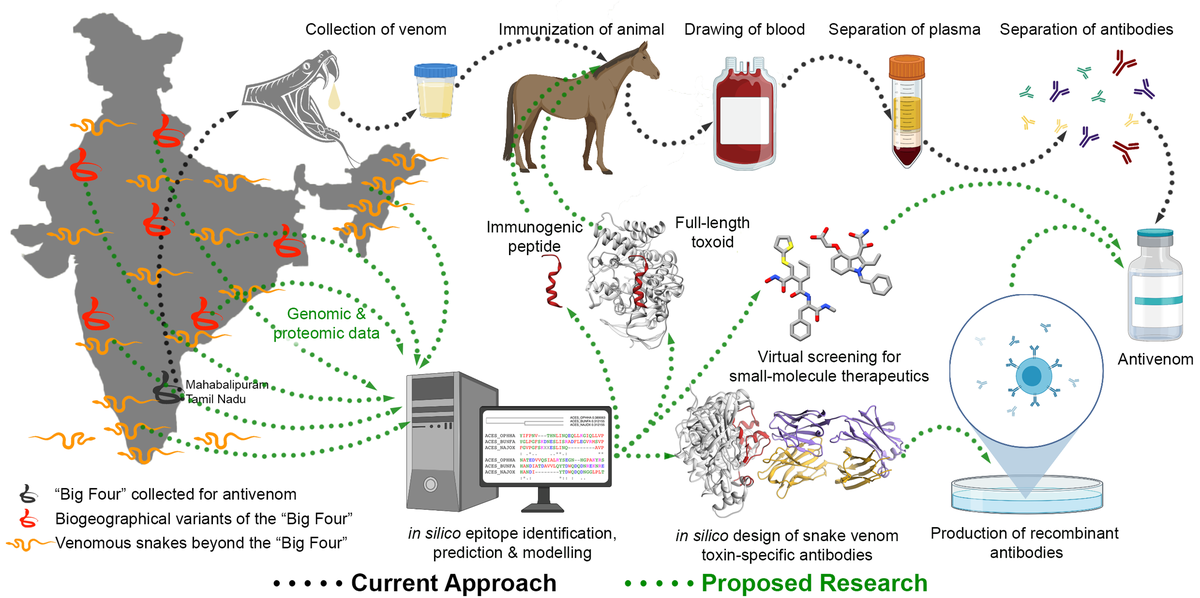
Polyvalent antivenoms (PVAs) currently used in India target multiple species. However, their efficacy varies against less common snakes. Understanding each venom’s complexity and the mechanisms of antibody production remains central to improving treatments.
How do antivenoms work?
The production of antivenom is a remarkable interplay of human ingenuity, animal resilience, and immunological mastery, dating back to the pioneering work of French physician Albert Calmette in the 1890s. He developed the first antivenom using horses, a practice that continues today.
To produce antivenom, healthy and mature venomous snakes are first captured from the wild by trained experts who then “milk” the snakes to extract the venom. Next, they immunise horses with increasing doses of venom over many weeks, allowing their immune systems to produce antibodies. The dose of venom injected into horses is critical: too little and the immune response will be weak; too much and the horse’s body could be damaged.
Over time, the horses develop a robust immune response, producing antibodies that neutralise venom toxins. The antibodies thus produced are very specific to the type of toxins injected, like a lock and its key. This process mirrors how humans develop resistance to familiar pathogens like the flu or common-cold viruses — through repeated exposure or vaccination. The experts extract these antibodies from the horse’s blood and purify and formulate them as antivenoms.
Several companies in India, including Bharat Serums and Vaccines, Haffkine Bio-pharmaceutical Corporation, and ViNS Bioproducts, produce antivenom this way. The Irula tribe of Tamil Nadu plays a crucial role in this process. The Irular people are skilled snake-catchers and can safely extract venom from snakes in controlled environments. Their expertise ensures a steady supply of high-quality venom for antivenom production in India. Without their contribution, the supply chain for these drugs would collapse.
How common is snakebite in India?
India is home to more than 300 species of snakes, of which more than 60 are venomous, ranging from mild to high. The so-called Big Four — Indian cobra (Naja naja), common krait (Bungarus caeruleus), Russell’s viper (Daboia russelii), and the saw-scaled viper (genus Echis) — account for most snakebite deaths. The venom extracted from these four species is used to produce PVAs in India.
On the flip side, this means other venomous snakes — including the king cobra, monocled cobra, banded krait, Sochurek’s saw-scaled viper, hump-nosed viper, and several species of pit vipers — are not covered by existing PVAs and continue to pose significant risks. As a result, victims bitten by these species often receive ineffective treatment, leading to poor outcomes.
A landmark 2020 study by researchers from Canada, India, and the U.K. estimated that between 2001 and 2014, a horrifying 1.2 million snakebite deaths and three-times as many cases of permanent disability occurred in India. The study also said one in 250 Indians were at risk of dying from snakebite before the age of 70.
These staggering mortality numbers reflect a pernicious combination of ecological, social, and systemic factors. People in rural India like agricultural workers are disproportionately affected and face a constant threat, particularly during the monsoon, when snakes become more active. Rapid, often unplanned urbanisation, poor garbage management, and urban floods have increased encounters between humans and snakes, making even city-dwellers vulnerable.
Why are antivenoms hard to get?
India is the world’s largest producer and consumer of antivenoms in the world. However, access to timely medical care remains a significant challenge for many Indians. People in remote areas often undertake long journeys to reach a healthcare facility equipped with antivenoms.
Even when antivenom is available, improper administration and inadequate facilities exacerbate the crisis. Logistical issues, unequal access to care, superstitious beliefs, and cultural practices often delay proper treatment in many parts.
Antivenoms often need to be transported in cold storage, however, India’s rural parts lack the supporting infrastructure and power supply. Facilities that ‘make do’ with the resources available can cause the antivenoms to degrade in storage and become ineffective.
The high cost of manufacturing antivenom limits accessibility for the economically-disadvantaged. This mismatch highlights the need for tailored solutions, underscoring the importance of targeted research and innovation.
How are antivenoms changing?
Antivenoms of the future are more promising. Researchers are using recombinant DNA technology to produce lab-engineered, synthetic antivenoms that are free from animal-derived proteins and offer greater safety and efficacy. Computer-designed proteins could accelerate development by helping researchers to optimise antibodies for different clinical settings.
For example, on January 15, researchers from Denmark, the U.K., and the U.S., led by 2024 Nobel laureate David Baker, reported successfully using Artificial Intelligence (AI) to design synthetic antivenoms. Their and other breakthroughs promise greater effectiveness, availability, and the potential to replace century-old methods to produce antivenoms.
Region-specific antivenoms are another promising avenue. The work of Karthik Sunagar at the Indian Institute of Science, Bengaluru, has already shed light on cross-species and geographic variability in venoms.
By mapping the toxins’ compositions, scientists are attempting to create tailored antivenoms, holding the promise for more precise treatments. Portable venom-detection kits and rapid diagnostic tools are also helping guide effective antivenom use. With continued investment in research, public education, and infrastructure, India can address its snakebite crisis, with reason to hope tragedies like Mayuri’s will become a thing of the past.
R.N.V. Krishna Deepak studies snake venoms using computational methods at Azim Premji University, Bengaluru.
Published – January 22, 2025 08:30 am IST

