When we talk about cardiovascular diseases, we refer to diseases of the heart and the blood vessels. While we know that the heart is a vital organ that pumps blood to the entire body, we should understand a few facts about blood vessels.
Blood vessels circulate oxygen, nutrients, hormones, and much more, and maintain the body’s homeostasis, that is, a stable internal environment despite changes in the external environment. The collective length of the entire vasculature, including arteries, veins, and capillaries, is approximately 96,000 kilometres in a human adult! The thin inner lining of the blood vessels, called the endothelium, is an important endocrine organ regulating the body’s metabolism, immune response, inflammation, coagulation, and blood flow. By caring for the health of our blood vessels we are indirectly caring for all our organs and our overall health.
The term blood pressure, or BP, refers to the force of blood flow in our arteries, produced by the pumping action of the heart. Normal BP is less than 120/80 mmHg in healthy adults; values above this are classified as elevated, hypertension stages 1 and 2, and a hypertensive crisis based on the level of deviation from normal. Both BP and heart rate are vital parameters that help us understand the cardiovascular health of a person. More so, how one’s BP and heart rate respond to exercise is an important indicator of a person’s exercise capacity and fitness level.

The ‘deadly triad’
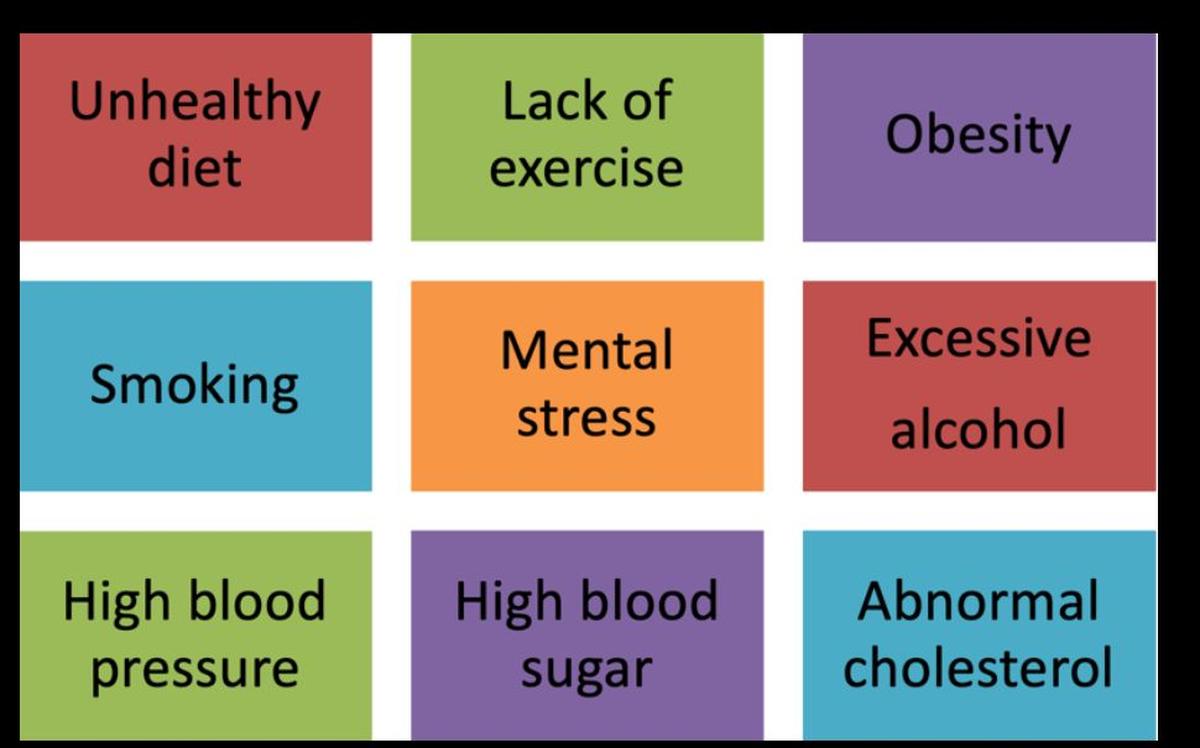
Hypertension or elevated blood pressure is one of three silent killers ravaging the health and well-being of people today. Together with diabetes and cholesterol imbalance, hypertension forms the ‘deadly triad’ that creeps up on us without any symptoms to cause a myriad of cardiovascular diseases (CVD) such as heart attacks, heart failures, strokes, and sudden cardiac deaths, as well as other organ damage such as kidney failure, liver dysfunction, loss of vision and dementia. Heart attacks and strokes are amongst the major noncommunicable diseases (NCDs) causing premature deaths in the current era. When the health of our blood vessels is compromised, they become a nidus for plaque build-up or atherosclerosis, ultimately causing coronary artery disease and heart attacks or cerebral artery disease and strokes. There are nine modifiable risk factors for heart attack as shown in Figure 1.
Figure 1. Risk factors for coronary artery disease
Hypertension poses an enormous burden to the health economy of our country as almost one in four men and over one in five women are hypertensive. Recent research has shown that a very high proportion of patients (around 53%) are unaware that they have high BP. On the other hand, the number of hypertensive patients who have their BP under control is abysmally low, around 20%. Rural India is unfortunately fast catching up with urban India in the high prevalence of all NCDs including hypertension. The loss of productive life-years due to hypertension, and the cost of hospitalisation and treatment of CVD and other NCDs is so high that the only way out of this vicious cycle is to improve awareness about hypertension and empower people with simple and cost-effective strategies to prevent it.
Causes and prevention strategies
The story of how hypertension develops is long and complex, the main characters being too much salt in our diet, inadequate fruits and vegetables, excessive saturated fats and trans-fat, lack of exercise, abnormal body weight, poorly managed stress, lack of sleep, tobacco use, and alcohol consumption. Genetic factors, environmental pollution, ethnicity and age act as supporting characters in the hypertension plot. The moral of the story is simple: the lifestyle choices we make on a daily basis are the biggest contributors to the development of hypertension.
The key steps to curbing the growing incidence of hypertension are:
-
Making healthy lifestyle choices daily
-
Resetting unhealthy behaviours/other risk factors on a weekly basis
-
Getting BP checked monthly (in hypertensive individuals) or yearly (in normotensive individuals)
-
Getting a cardiovascular assessment regularly as advised
-
Following a comprehensive lifestyle modification programme (for at-risk individuals) or a cardiac rehabilitation programme (for heart patients)
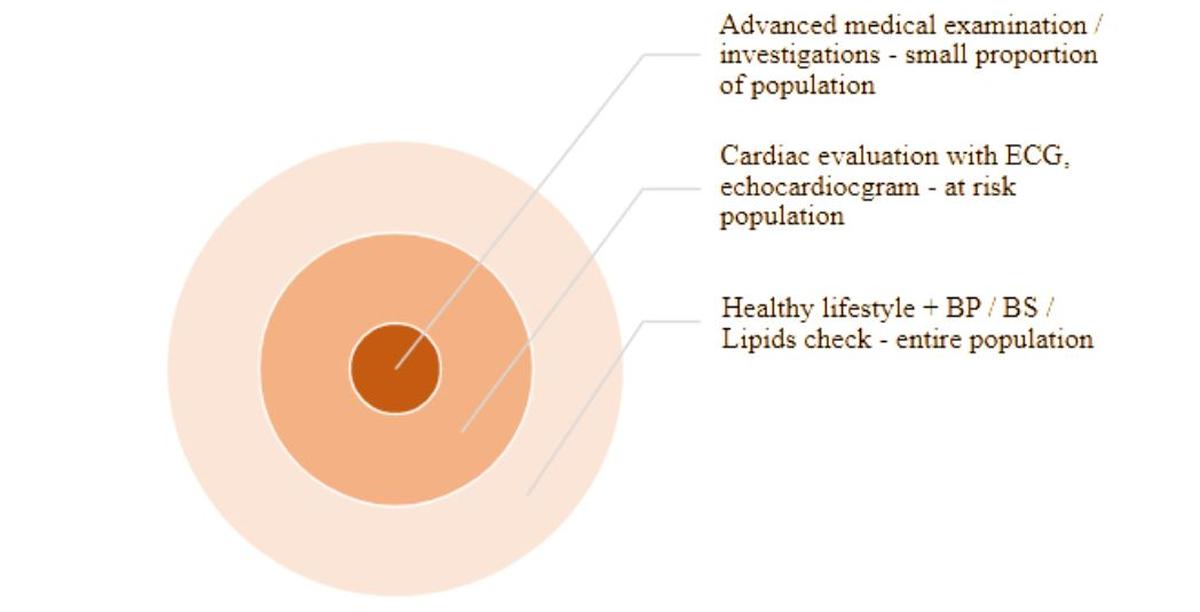
What this means is that all individuals should have their first health-related lifestyle assessment along with BP, blood sugar (BS) and lipids checked at the age of 20 and thereafter every five years, moving to annual checks from the age of 40 onwards.

Figure 2 outlines the population-level approach for hypertension prevention through lifestyle changes and medical examination.
Figure 2. Population-level approach to prevent hypertension
Lifestyle mantras to prevent hypertension
What to eat? At least five portions of vegetables and fruits, at least 1-2 portions of whole grain dishes, adequate proteins and limited healthy fats daily; limiting salt while cooking at home and avoiding packaged/ready foods; the healthy eating plate concept should be followed for every meal.
How to prepare the meal and eat it: Prepare meals at home as much as possible, eat food mindfully, slowly and enjoy every bite, and have at least one meal a day with family members/ friends. Eat when hungry or work up an appetite before sitting for a meal, and finish eating at least 2-3 hours before bedtime.
Is exercise a must? Regular exercise, at least five days a week, is a must for all, irrespective of whether you are physically active throughout the day or not. At least 30 minutes of brisk aerobic exercise five days of the week (total of 150 minutes) and strength training two days of the week are mandatory for all; intersperse every 30 minutes of a sedentary period with five to 10 minutes of activities such as stretching, brisk walking, stair climbing or workstation exercises; remember, “sitting is the new smoking”.
What type of exercise is needed? A combination of aerobic exercises (brisk walking, cycling, swimming, jogging, dancing), strengthening exercises (using equipment or weights), flexibility exercises (yoga, tai chi), and balance exercises should be followed by all.
How to manage stress? Stress management techniques such as meditation, deep breathing, regular exercise, and active hobbies (dancing, gardening, sports, creative arts) should be practised on a daily basis to keep stress at bay.
Is sleep a risk factor? Lack of sufficient and good quality sleep can cause hypertension; aim for 7 to 9 hours of undisturbed sleep daily.
Is tobacco harmful? Tobacco use in any form (even passive smoking) is an important risk factor for hypertension, heart disease and stroke; quitting tobacco completely is the best gift of health to oneself; professional help may be sought to quit tobacco use.
Is alcohol good or bad for the heart? Alcohol in any form is harmful to the body; excessive/binge alcohol consumption can lead to hypertension and other ailments and should be avoided.

Early detection of hypertension
Effective population screening programmes are the ideal way to identify hypertension early. As the age cut-off for initial CVD screening is 20 years, basic health screening with BP measurement should become mandatory in all higher educational institutions as well as a criterion that employers must implement. Individuals who do not fall under either the formal education system or employment channels should be screened by innovative strategies such as while appearing for their driving licence or voter ID issuance.
As a single reading of high BP is not sufficient to diagnose hypertension, those with an elevated BP should be referred to a physician for a further physical examination and structured BP evaluation. It is important to rule out medical causes of hypertension such as kidney disease, endocrine abnormalities, arterial disorders and sleep apnoea before arriving at a diagnosis of primary or essential hypertension.
Adequate control of hypertension
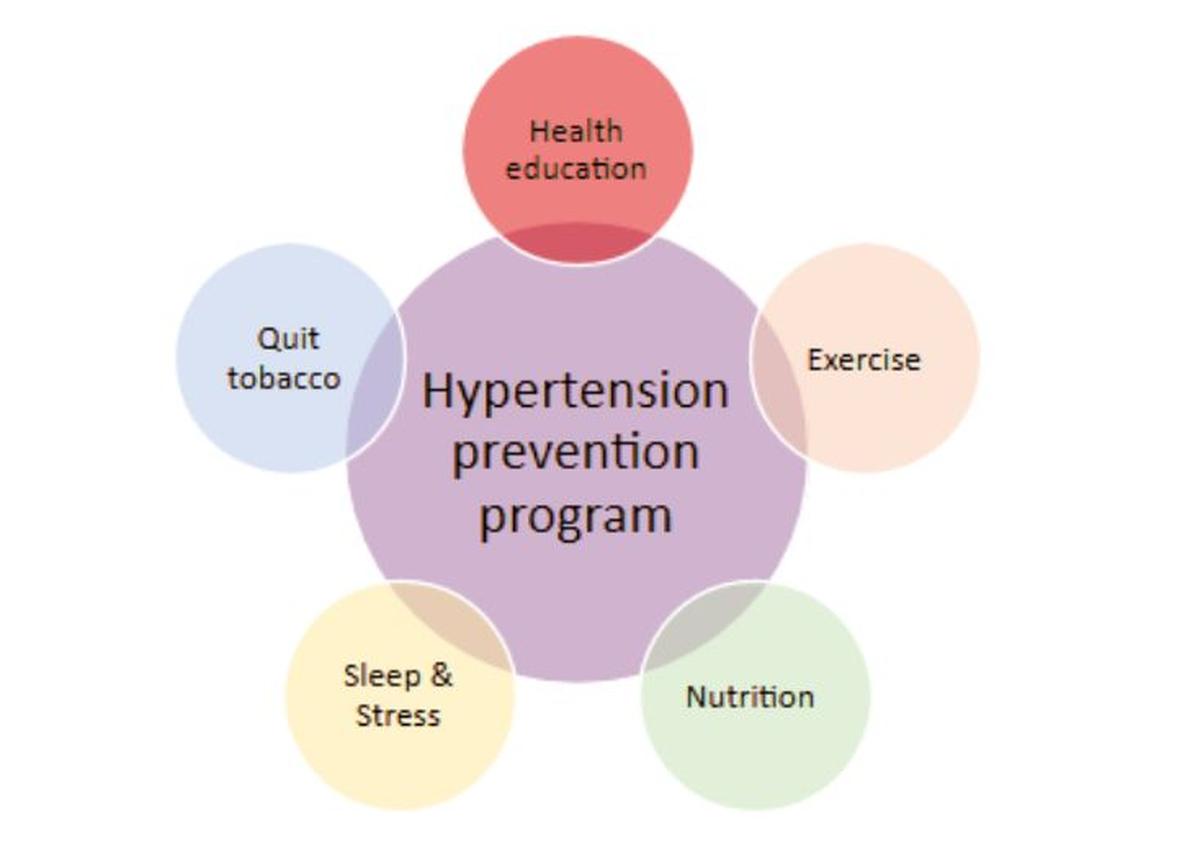
Once someone is diagnosed with mild to moderate hypertension, a personalised approach to modify the causative lifestyle habits should be tried first. A comprehensive CVD prevention programme provided by a multidisciplinary team of healthcare professionals and comprising education, exercise, nutritional and psychosocial interventions has been proven to reverse elevated BP in a vast majority of newly diagnosed hypertensive patients. A close watch on the BP trajectory and close supervision of the adherence to lifestyle changes are mandatory during this three to six-month intensive lifestyle modification phase.
A poor response to the above step or a very high BP at initial diagnosis should prompt the initiation of BP-lowering medications, choosing either one drug or combination therapy, taking into consideration the individual’s clinical and sociodemographic background. The crucial thing in pharmacotherapy is once again frequent BP checks and fine-tuning of the type and dosage of the drug(s) to achieve target BP with as few side effects as possible.
Non-compliance to drug therapy being the commonest cause of poor BP control, medication education is key to ensuring adherence to the prescription. Both the physician and the patient should take joint responsibility in achieving the target BP through a health plan that is drafted for the patient and by the patient, with the physician’s expert help.

Figure 3. Components of a multidisciplinary prevention programme
Preventing organ damage
As hypertension, just like diabetes and cholesterol imbalance, is known to cause multi-organ damage, constant surveillance for heart disease, impaired kidney function, vision abnormalities, fertility issues, and lung disease is a must. Early detection of signs of organ damage will enable referral to specialist care and escalation of medical management to stall the damage and potentially reverse it. Just like a multidisciplinary prevention programme helps reverse hypertension, a comprehensive cardiac rehabilitation programme is key to addressing the multipronged needs of individuals with heart disease and reversing their disease process.
For a preventive cardiologist, the biggest medical challenge today is managing individuals with multimorbidity, a combination of conditions such as hypertension, diabetes, cholesterol abnormalities, obesity, chronic lung disease, fatty liver, impaired renal function, poor mental health, and heart ailments. Elderly patients with frailty, musculoskeletal issues, and weakened immune systems are even more difficult to treat when they have multi-organ damage.
While medical and surgical therapy should be deployed as and when deemed necessary, in addition to medication, reinforcing the building blocks of a healthy lifestyle will help improve functional status, quality of life, and resilience to infections at any stage in the disease spectrum.

The way forward
A close collaboration amongst all stakeholders, namely the public, healthcare professionals, and policymakers, is important, moving forward, to halt the hypertension epidemic before it becomes an untameable beast. Epidemiological, basic scientific and clinical research should progress hand in hand to help us unravel some of the persisting dilemmas and challenges in the domain of hypertension, CVD and NCDs. In this era of superpowers, each one of us should recognise the superpower within us, our mind, that is capable of adopting health-promoting habits and adapting to the changing environment to protect our health and well-being. The collective power of our minds in changing the course of deadly diseases should also be harnessed through education, awareness and adherence.

Myths around hypertension
Myth 1: I am feeling fine and hence do not see the need for a BP check.
High BP usually does not cause any symptoms. In other words, individuals who are feeling fine can still have hypertension and should get their BP checked.
Myth 2: Hypertension is in my family and genes and there is nothing I can do to prevent it.
While genetic factors play a role in the causation of hypertension, there is scientific evidence to show that healthy lifestyle choices can overrule genetic predispositions and protect us from the disease.
Myth 3: Once diagnosed, hypertension is a lifelong disease.
Early diagnosis can help reverse hypertension through lifestyle changes and prevent end organ damage.
Myth 4: If my BP comes down with medicines, I can stop taking the pills.
BP medications should not be modified or stopped without the advice of your physician.
Myth 5: I don’t have to watch my diet or exercise when I am on BP medication.
It is extremely important to lead a healthy lifestyle even while on BP medications, as otherwise your hypertension will worsen, become resistant to treatment and lead to end organ damage within a short time.
(Dr. Priya Chockalingam is the clinical director, Cardiac Wellness Institute, Chennai.)
Published – May 28, 2025 04:30 pm IST

